Related articles
Read more
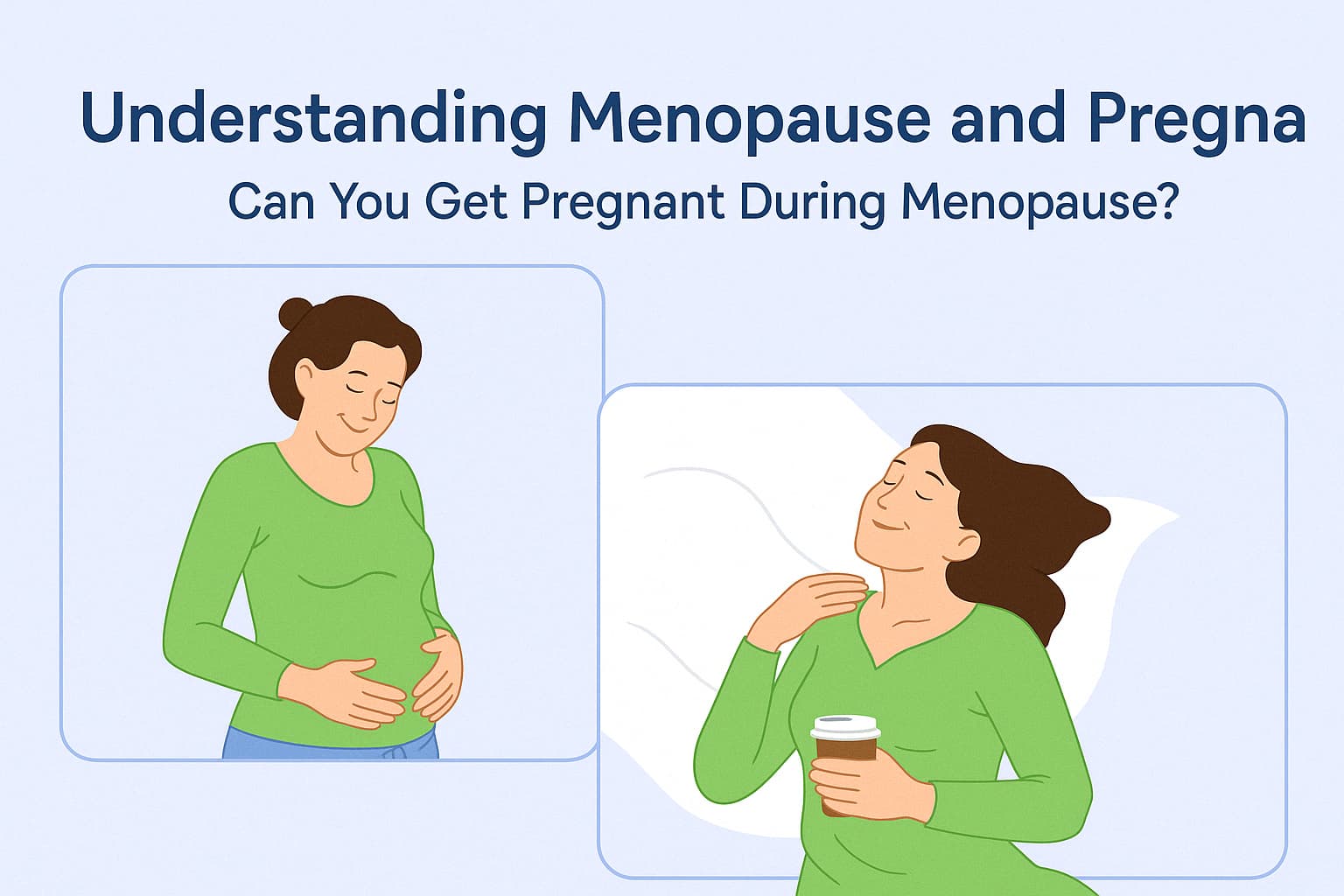
Menopause marks a significant transition in a woman’s reproductive life, typically occurring between the ages of 45 and 55, with an average onset around 51. It is defined as the permanent cessation of menstruation for 12 consecutive months due to the decline in ovarian function and hormone production, particularly estrogen and progesterone. However, the possibility of Pregnant During Menopause, as well as during premenopause or perimenopause, is a common concern, as is distinguishing between menopause and pregnancy symptoms. This article explores these topics comprehensively, addressing fertility, premature menopause, assisted reproductive technologies, and practical tools for tracking symptoms.
Menopause is the point when a woman no longer has menstrual periods, signaling the end of natural ovulation and fertility. Women are born with approximately 1–2 million immature eggs, which decrease over time to about 26,000 by age 37. By menopause, the ovarian reserve is nearly depleted, and the ovaries stop releasing eggs.
Perimenopause, the transitional phase leading up to menopause, can last 4–10 years and is characterized by irregular periods, fluctuating hormone levels, and symptoms such as hot flashes, night sweats, mood changes, vaginal dryness, and urinary issues. During perimenopause, ovulation becomes unpredictable but can still occur, making pregnancy possible.
Premature menopause, also known as primary ovarian insufficiency, occurs before age 40, affecting about 1% of women. It can be caused by genetic factors (e.g., Turner syndrome), autoimmune disorders, chemotherapy, radiation, pelvic surgeries, hypothyroidism, smoking, or polycystic ovary syndrome (PCOS). Symptoms mirror natural menopause but may be more intense due to the rapid hormonal decline.
Menopause and pregnancy share overlapping symptoms, especially during perimenopause, making differentiation challenging. Common shared symptoms include:
Women over 35 trying to conceive for 6 months, or those over 40, should consult a doctor promptly if conception is delayed, as fertility declines rapidly with age.
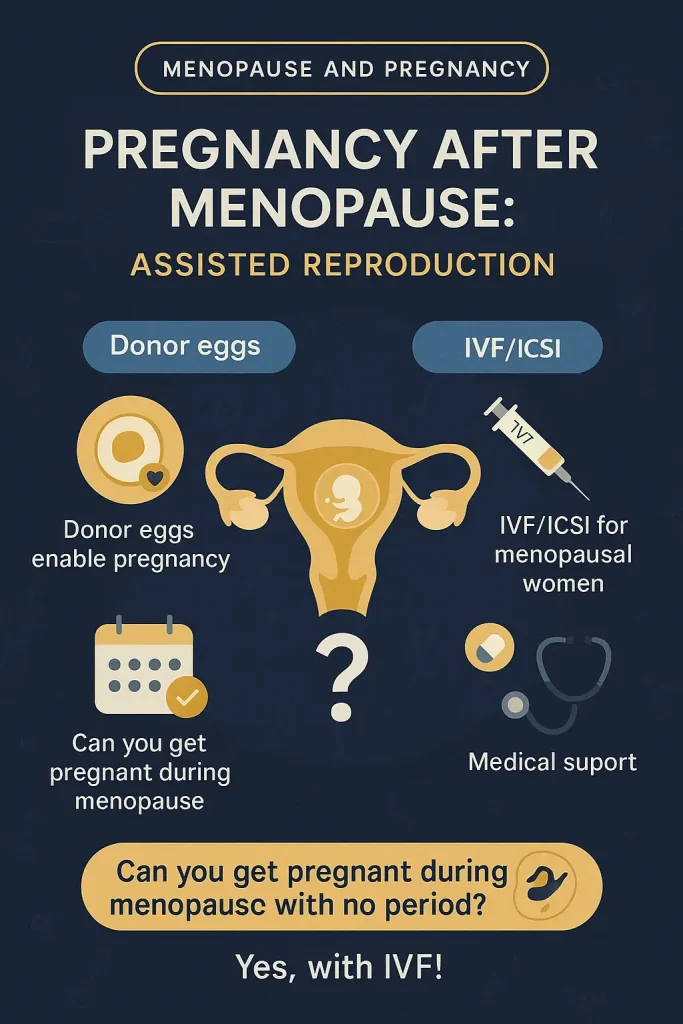
Pregnancy after 45, whether natural or via IVF, is high-risk due to:
Women should undergo thorough medical evaluations and consult fertility specialists to assess risks and explore options like donor eggs or preimplantation genetic testing.
After menopause, decreased estrogen levels increase the risk of:
HRT, calcium supplements, weight-bearing exercise, and a heart-healthy diet can mitigate these risks. Regular medical checkups are essential for early detection and management.
Menopause in one’s 20s is extremely rare and usually linked to premature menopause caused by genetic conditions, autoimmune disorders, or medical interventions. Women experiencing symptoms in their 20s should seek immediate medical evaluation to identify causes and explore fertility preservation options, such as egg freezing.
For women navigating menopause or considering pregnancy, consulting a healthcare provider or fertility specialist is crucial. Tools like cycle-tracking apps and timely medical evaluations can provide clarity and support informed decisions.